First things first: shout out to my older brother for posing the question responsible for today’s post – and the
playlist that I’m blogging to! Now, onto the actual discussion.
Blue Light
Blue light is a topic that’s received a lot of attention in (relatively) recent years. I briefly mentioned blue light in my post Specs: Do I Really Need… For a more complete discussion on this topic though, we need to do a quick physics/optics review.
First things first: light functions as a wave… and a particle. Which is admittedly a bit confusing – until you think about the two ways that light can be defined: by how it travels (in a wave), and the energy that it carries (as a particle).
As a wave, it falls in the electromagnetic spectrum – along with a lot of other familiar things like:
- gamma rays
- x-rays
- ultraviolet
- infrared
- microwaves
- radio waves
Collectively, these are all types of radiation.
Which can be a scary term. I mean, it’s easy to think of radiation in the context of cancer – both as a cause and a treatment.
However, while radiation gets a bad rap, in its most basic definition, radiation is simply traveling energy that spreads out as it goes.
From there, each type of radiation presented above, including visible light, which falls right between ultraviolet and infrared light, has slightly different properties in regards to wavelength and energy. For instance, gamma rays have short waves, but a lot of energy (higher frequency), while radio waves, on the other hand, are longer waves with less energy. (Yes, the list went in order!)
Practically, what does this mean?
Well, the more energy something has, the more tissue it can penetrate and the more damage can ensue. This is a specific concern in relation to the human body. When more energy is introduced into the system, it can cause changes on the cellular level. A relatively low amount of radiation for a short period of time doesn’t necessarily cause irreparable damage, but the higher the dose or the longer the exposure, the greater the risk.
Let’s jump back to visible light.
Due to its duality, visible light can be defined in two ways: wavelength and frequency. In regards to wavelength, light is typically visible to the human eye from ~380-700 nanometers. This corresponds with a frequency of 4-8 cycles/second (aka Hertz).
If we bring your elementary art class into the mix, you’ll remember that electromagnetic radiation isn’t the only spectrum we’re looking at – visible light is also made up of a spectrum: ROY G BIV. Fantastically, this list is in order of wavelength and frequency, with red at the longest wavelength, and therefore the lowest frequency/energy, and blue on the opposite end of the spectrum (closest to UV rays) with the shortest wavelength and highest frequency.
Initially, it was the high(er) energy nature of blue light that brought cause for concern.
Okay, time for a tech lesson (which, in theory, I’m probably not the most qualified to give, but let’s see what happens.)
Throughout the years, there have been a number of different types of light-bulbs – from the incandescent, in which the filament is heated until it glows, to the fluorescent, which uses argon and mercury to produce UV light that stimulated the phosphor coating to emit visible light, to the increasingly popular light emitting diode (LED), which transmits electricity through a semi-conductor to produced light.
Each of these light-bulbs, due to the difference in functioning mechanism, produces different levels of light throughout the visible spectrum. For instance, incandescent bulbs produce “warmer” light, with a lower energy profile (since most of the energy is lost as heat). LED lights, which were designed for energy efficiency, are on the opposite end of the spectrum, with a cool light profile.
Prior to LEDs, most screens used traditional fluorescent lights, as part of liquid crystal displays or LCDs. As fluorscents are less efficient than LEDS (though more efficient than incandescents), more energy was lost in the process of light production. Most screens today, however, use LEDs, which emit (or at least initally emitted) more blue light than traditional fluorescent lights used in LCD monitors.
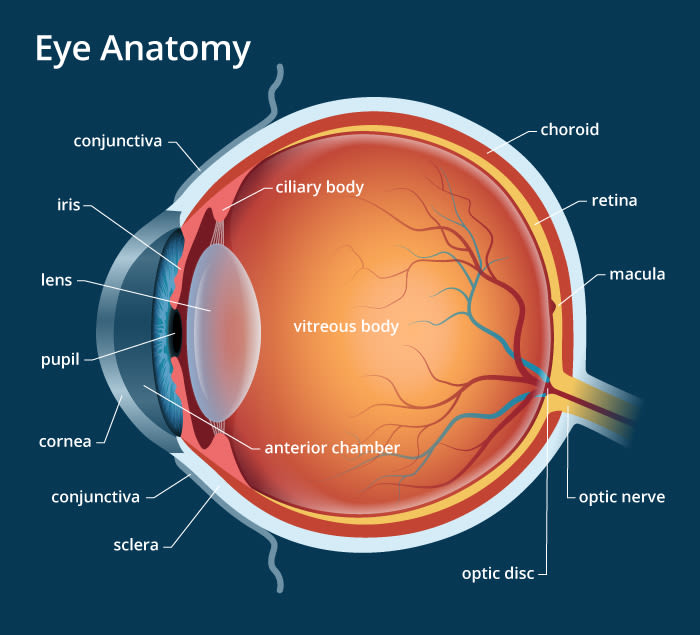
With this in mind, the greatest fear associated with the LED transition was that (excessive) screen use would increase blue light exposure to a toxic level that would cause permanent damage to the eyes (specifically the macula, or the most central portion of the vision).
However, in recent years, this theory has (largely) been disproved.
Why?
Because screens, monitors, or even other LED lights in your house or workspace, come nowhere close to emitting the same levels of blue light that another source of light that people have been exposed to since the dawn of time creates.
What is this source?
The sun.
So, then, what’s the problem with blue light?
Great question! There are a couple of current theories, however, for the sake of post length, I won’t dive into them today. If you’re interested, be sure to check back for Part 2 to find out!
If you have any questions or comments, please contact me! If you’ve enjoyed this article, please subscribe, or like my page on Facebook!